 Open wechat
Open wechatDifferential diagnosis of periapical cysts and odontogenic cysts
1. Dentistry cyst
Dental cysts account for 24% of true cysts in the jaw, and the incidence of permanent teeth is second only to periapical cysts, and deciduous teeth are rare. More common in 20~30 years old unbud permanent teeth, wisdom teeth, multiple teeth or dental tumor. 75% occurred in the mandible, and the incidence of mandibular third molar was 45.7%, followed by maxillary permanent cusp, mandibular premolar, and maxillary third molar. A.Dhupar et al reported that the incidence of maxillary premolar with dental cysts was only 2.7%. Most single cysts are extremely rare (except developmental syndrome, systemic disease or certain drugs). A. [] Dhupar et al summarized the English literature from 1943 to 2017, only 30 cases of bilateral dental cysts were reported, 3 with maxilla, 24 with mandible, and 3 with both upper and mandible. The mouth may be accompanied by missing teeth or more than one teeth, the cystic fluid is grass yellow or grass green clear liquid, see cholesterol crystals under the microscope. X-ray shows the crown in the transmission area of the jaw, and the root is not completely formed. The capsule wall is attached to the line of the enamel cementum.
2, glandular dental origin cyst
Adenular odontogenic cyst is a benign, rare odontogenic developmental cyst.Magnousson et al reported that out of 5800 cysts, only 7 were odontogenic cysts. More common in 45 to 50 years old, 70% occurred in the front of the mandibular region, the diameter ranged from 1 cm to different sizes. Cystic fluid is usually water sample and low viscosity liquid, X-ray film is follicular transmission projection, single or multiroom, well-defined (hardened edge). Small lesions are asymptomatic, while large lesions can have local enlargement, pain, paraesthesia and secondary infection. It is recommended to remove the affected teeth and follow-up for at least 3 to 7 years. This disease is locally invasive with high recurrence rate, and must be differentiated from odontogenic keratocyst, amelocylastoma and apical cyst. Therefore, preoperative biopsy is recommended to make a clear diagnosis.
Differential diagnosis of periapical cysts and non-odontogenic cysts
1, the rhinopalatine duct cyst
Rhinopatatal duct cysts are the most common non-odontogenic cysts. Accounting for 1.3%~4.2% of non-odontogenic tumors, which is more common in men aged from 30 to 40 years. Less invasive, low recurrence rate, and self-limited growth.Grossman et al reported that in 2905 cysts, apical cysts represented 61%, 25.3%, 7.2%, and 2.2% of rhinopatatal cysts 2.2%. The clinical manifestations are mostly the uplift of the incisor papillary area, with different sizes and clear borders. The X-ray shows a circular or heart-shaped transmission projection between or behind the roots of the two upper central incisors. The best treatment method is surgical removal, and pathological examination is required for the diagnosis.
2, and the ectopic meningioma, where no
Ectopic meningioma is a rare disease, with only 8 cases reported worldwide (2 maxilla and 6 mandible). Elderly women are common, imaging examination is not specific, used to understand the relationship between tumor and jaw, and exclude malignant lesions. Frequent surgical removal. For the unknown damage to the jaw bone, a biopsy should be done.
case
Basic information patient Tan, male, 54 years old. Main complaint of anterior hard palate mass for more than 10 days.
Medical history: the anterior mass of the hard palate was found 10 days ago, without significant pain. He went to a local hospital, with pus on puncture, and was diagnosed as "cyst and infection". The mass shrank after oral anti-inflammatory drugs. The patient fell down while cycling 2 years ago and broke his front tooth untreated.
Past history: no special items.
Intraoral examination: 11 enamel crack, lip and dark yellow crown, loose I°, no response to electrical vitality test. 121 / 3 of the crown transverse broken, crown color dark yellow, loose I°, electrical vitality test no response. 13 Dental color was normal, and the electrical vitality test was normal. 11~13 Palatal lateral mucosa swelling, fluctuation of touch, without tenderness. See light yellow cystic fluid for puncture, see very fine shiny particles inside, curved body layer sheet and CBCT as shown in Figure 1.
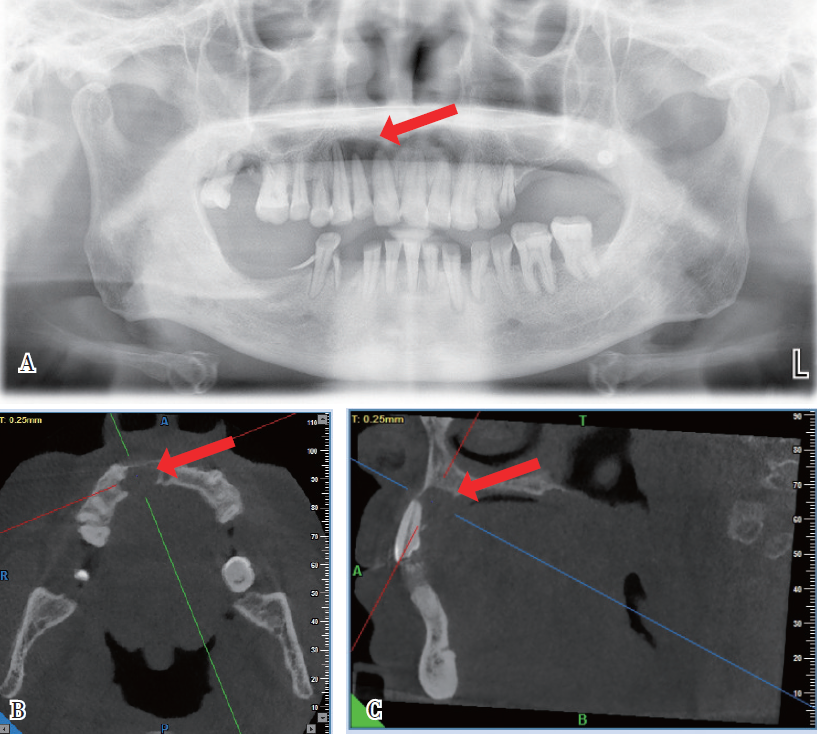
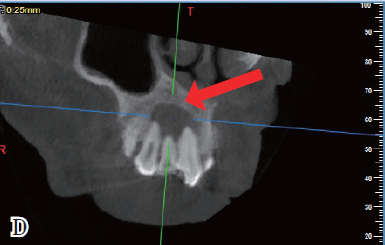
Figure 1 Case 1 initial slice, A is curved layer; B is CBCT axial, C is CBCT sagittal, and D is CBCT coronal
Clinical diagnosis: 11,12 apical cysts.
Treatment: All operations were completed under the microscope after the upper rubber barrier. 11,12 Open pulp on the side of the palate. Both are single tubes, 12 working length 19 mm, 11 working length 21.5 mm (flat rim).Reciproc Single file 25 #, ProTaper hand clean with file 30 # root tube, ultrasonic and wash with distilled water for 3 hours. When the root tip exudate decreases significantly, wipe the root canal and seal the calcium hydroxide paste.
Second visit: 4 days later, temporary sealing and root canal calcium hydroxide paste, wipe dry, 12 see the reflective fluid surface, 11 no exudate, 1% sodium chloride ultrasonic wash for 2 h, to 12 tubes, wipe the root canal, and reseal the calcium hydroxide paste. After 2 weeks, 11,12 tubes without exudate, the test tip (Figure 2) after appropriate, 5.25% sodium hypochlorite rinsed, Nd: YAG laser disinfection, dried the root tube, AHplus paste + hot tooth gum vertically pressurized to fill the root tube, the flow resin was closed, the crown pulp cavity Z350A3 filled and polished. CBCT after 3 months, the apical shadow was significantly reduced (Figure 3). The CBCT review after 10 months showed only a little shadow on the root tip (Figure 4).
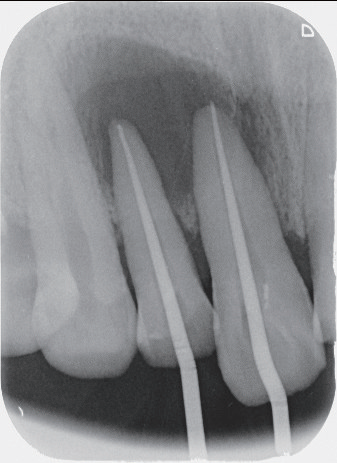
Figure 2 Case -21,22 tip tip
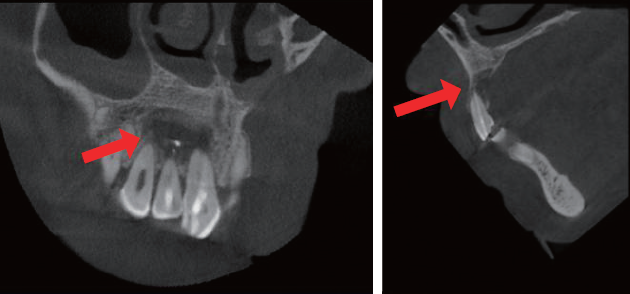
Figure 3: Case 1:3 months after surgery
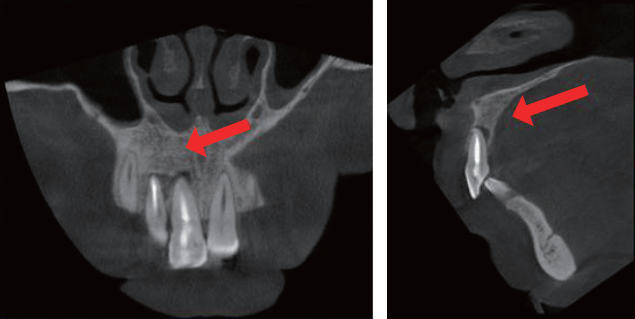
Figure 4: Case 1:10 months after surgery

